A CERDIGION father who suffered a stroke when he was just 31-years-old is calling for more specialist mental health support in the region.
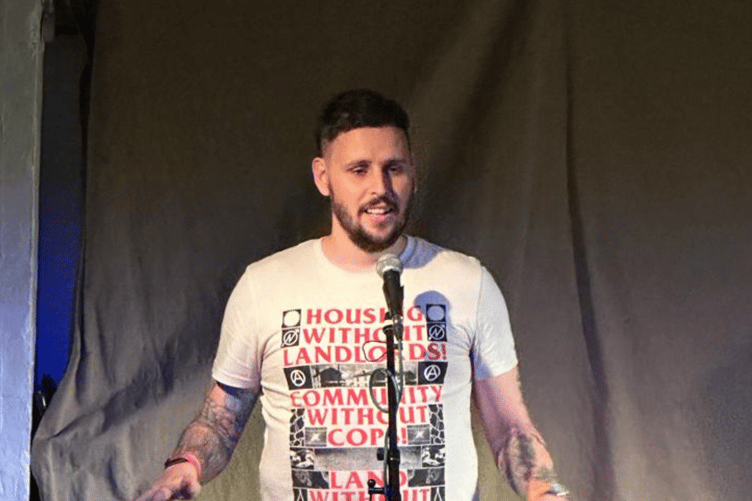
Father-of-two, Aaron Kent, 35 years old from Talgarreg, Llandysul had a stroke in October 2020.
His wife Emma was told to plan her husband’s funeral as most people who turn up at hospital in his condition don’t make it. The father of two young children, Otis 9 months old and Rue, 3 years old at the time did pull through but the recovery journey has been a difficult one.
“The most painful decision I ever made was to die. I had been out of a coma for about three days when it became clear how complex and difficult the journey ahead of me would be, not just for me but for my loved ones; I came to the conclusion that rather than burden them with the difficulties of my recovery and post-stroke life, it would be easier to close my eyes and let death embrace me. This, unfortunately, is the stark reality of confronting the world after a stroke for many people.”
Aaron was a fit and healthy sport loving 31-year-old English teacher when he had a stroke. He had been teaching a GCSE lesson on MacBeth when his life changed forever.
“The class were engaged in quiet work when I had a pain like somebody had boiled a kettle, waited for it to whistle, then poured the scalding water over the crevices of my brain. I got cover for the class, walked to reception, asked for paracetamol, and woke up a week later. Looking back, this is the first point at which my mental health began to erode, at the point of diagnosis. Telling somebody they've had a stroke is not like telling somebody they've broken a finger. No, this carries with it a history of stigma, a culture of fear, and a premonition of a lonely path ahead.”

Before this, Aaron had had a prestigious career and life full of achievements. Aaron joined the military and served as a submariner at 20, became a teacher at a prestigious private school Llandovery College at 29 and was awarded a medal at 30. Now at age 31, recovering from a stroke, he was being guided to walk again, was unable to shower alone and was being assessed on his safety while making a cup of tea in a hospital kitchen. Aaron was in University of Hospital, Cardiff and Neath Port Talbot rehab unit for nearly six weeks, unable to see family because of the Covid-19 lockdown.
“When I left hospital, I became aware of how alone I was and felt. Emma was a rock and supported me wholly, but she had no first-hand experience of suffering a stroke. I reached out to stroke forums and Facebook groups, for some detached hand that could guide me in the dark, but the nature of distance meant a revolving cast of people came and went, all just as lost sharing their experience and trying to understand this new post-stroke world. I couldn’t lift my children, my vision was affected and every headache, flash of eye pain, spell of light-headedness was met by a stone-cold belief that I was suffering another stroke.
“My world changed entirely, everything I had taken for granted had to be reconsidered. And when I thought I had overcome the stroke, new issues would come up: panic attacks, fatigue, lifestyle changes. Whenever you feel you are free from the stroke it pulls you back in and reminds you that you are not who you were. The counselling never materialised, I sat on a waiting list for years, but got no luck. Every avenue I had tried was met with failure, failure on behalf of a duty of mental health care, and a systemic failure of post-stroke guidance.”
Today, Aaron is paying for private counselling, which he still has weekly, his business is successful as a writer, physical health besides vision loss is back to previous levels and he is able to do exercise again but the mental health struggles have not disappeared.
“I was putting my son to bed last August, when I suddenly felt the walls close in around me, and an undefinable impending sense of doom. I couldn’t confirm the feelings, but I was rapt by the idea that I was dying, that my brain was bleeding again, and I was about to die. I held my three-year-old son, and wondered if I would ever see him again, if he was about to watch his father die on his bedroom floor, if I were about to burden him with a memory no child deserves. Then it passed. The next day, as I prepared lunch, it happened again. This continued two to three times a day for the next week before my GP prescribed me beta blockers and told me I was having panic attacks due to PTSD from my stroke.
“Three years down the line and here it was again, rearing its head and controlling my life. I yearn for a future in which stroke survivors are walked out of hospital doors with a solution, and a pathway to recovery. A future where stroke survivors don’t say goodbye to their hospital bed and their mental health at the same time. And a future where a stroke isn’t the great unknown for survivors and family members alike, but a clear, concise, careful journey defined by the success of this mental health provision.”
Charities working together
Stroke Association and Mind Cymru have partnered to produce a report highlighting the need for stroke survivors to have specialist mental health and wellbeing support to help rebuild their lives.
Stroke survivors across Wales are missing out on much needed specialist mental health and wellbeing support, reveals a recent report by the Stroke Association and Mind Cymru.
When stroke strikes, part of your brain shuts down. And so does a part of you. That’s because stroke happens in the brain, the control centre for who we are and what we can do. Lives change in an instant. As a result, people who survive a stroke often experience significant mental health struggles, including depression, anxiety, mood swings, panic attacks and suicidal thoughts.
There are more than 70,000 stroke survivors living in Wales. Yet there is little specialised support available to help them address their mental health.
A recent survey conducted by the Stroke Association found that around three quarters of stroke survivors experience at least one mental health problem following a stroke. Yet only 3% received support when they needed it the most.
The Stroke Association currently offers ‘tier 1’ psychological support to address this gap; via support coordinators in the community, the helpline, peer support from other stroke survivors, and social activity groups. But there’s a gap in ‘tier 2’ support for stroke survivors struggling with mild/moderate depression and/or anxiety.
The report explored the lived experience of over 100 people across Wales including stroke survivors, loved ones of stroke survivors and those who work with stroke survivors. Further discussions with 12 stroke survivors found that people do not expect the negative impact on their mental health after experiencing a stroke so it comes as a shock. Stroke survivors also feel alone and uncertain in their recovery. It affects people’s identity, and they can struggle to adapt.
Katie Chappelle, Associate Director for Wales, Stroke Association said, “We know that there is no ‘silver-bullet’ solution for helping stroke survivors rebuild their mental health, yet we want to see mental health given the same attention as physical health when recovering from stroke. Working with Mind Cymru and people affected stroke, we have begun to develop ideas for solutions including a specialist wellbeing recovery group for stroke survivors. However, this idea needs funding if we are going to be able to adequately support people across Wales to rebuild their mental health after stroke.
“We’re calling on those who plan and provide health and social care to work with us to ensure that people affected by stroke receive quality, timely support for their mental health and wellbeing. We urge GPs, Health Boards and clinical staff across the NHS to recognise that identifying and managing mental health issues post-stroke are an essential part of clinical rehabilitation and long-term stroke recovery.
Recovery from stroke is tough, but with the right support and a ton of courage and determination, the brain can adapt. We want to support more people to adapt to their new life after stroke.”
Simon Jones, Head of Policy and Campaigns at Mind Cymru, said: “Recognising parity between physical and mental health is something that’s often talked about, but we still have a long way to go before equal focus and attention is afforded to both.
“Unfortunately, as Aaron’s experiences demonstrate, the knock-on impact to someone’s mental wellbeing of a major health condition such as stroke can be overlooked. All too often this means that people can experience patchy support for their mental health.
“It’s been really positive to work with the Stroke Association, local Minds and people with lived experience on raising awareness of this issue. In developing its next mental health strategy, we urge the Welsh Government to look holistically at physical health services and pathways, so that people are able to access complementary mental health support at the point of need.”





Comments
This article has no comments yet. Be the first to leave a comment.